Accelerating Cures by Three Stages of Care and Research
The Stroke & Applied NeuroScience Center is committed to improving the lives of our patients before, during, and after hospitalization for stroke and other neurological conditions.
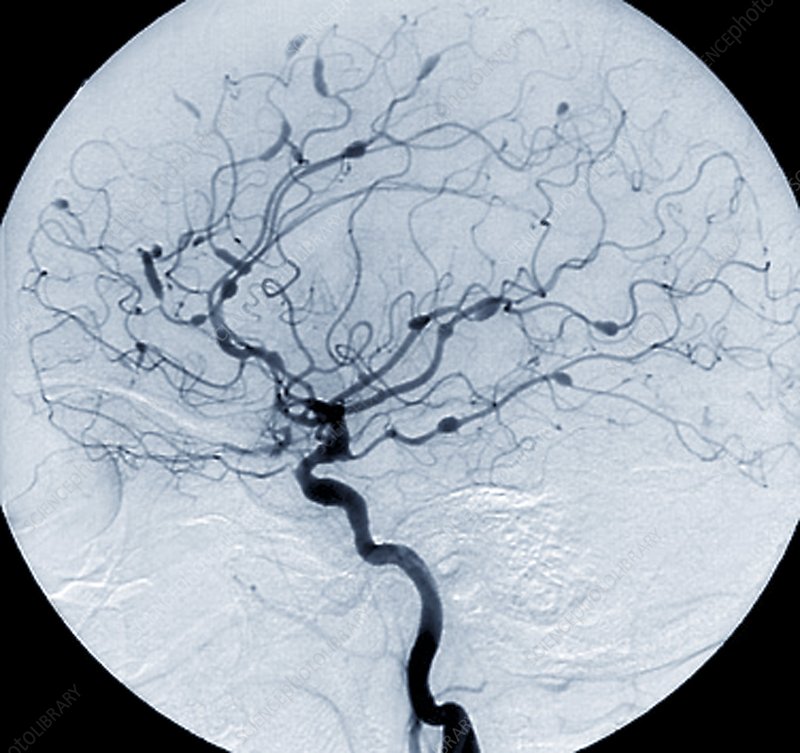
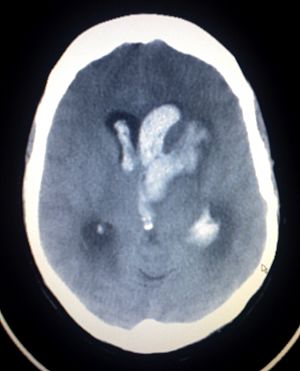
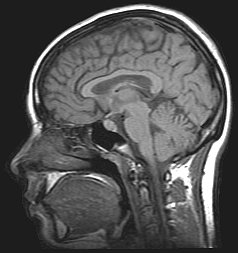
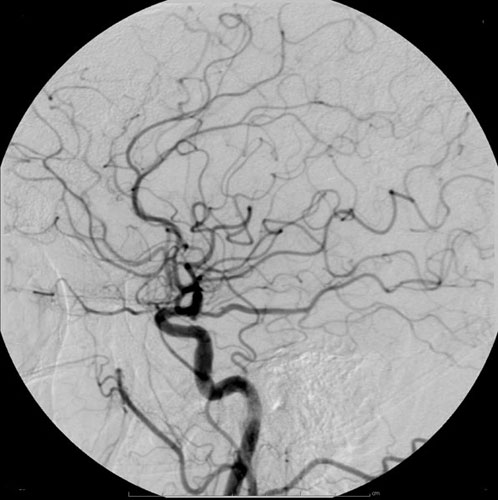
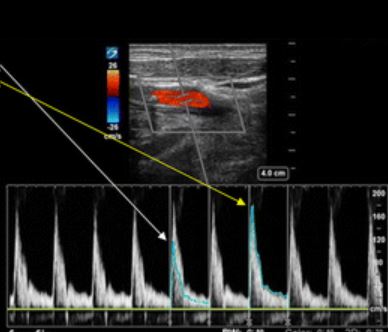
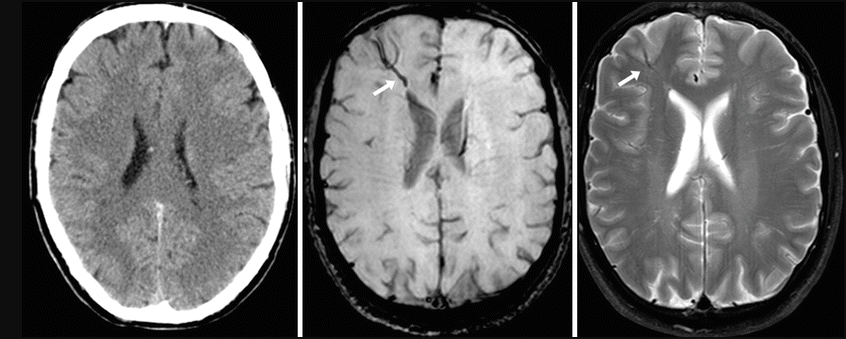
BEFORE:
Develop early detection and diagnosis to understand the the underlying cause of stroke and other neurological conditions through novel minimally-invasive techniques and machine learning.
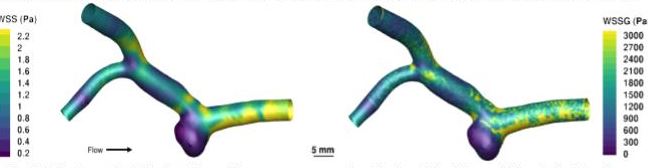
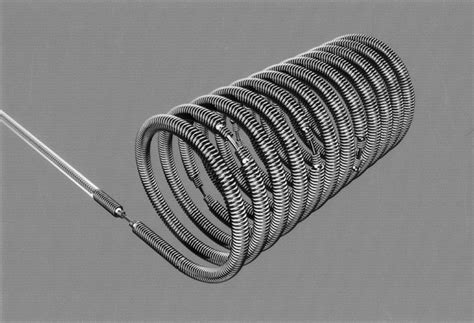
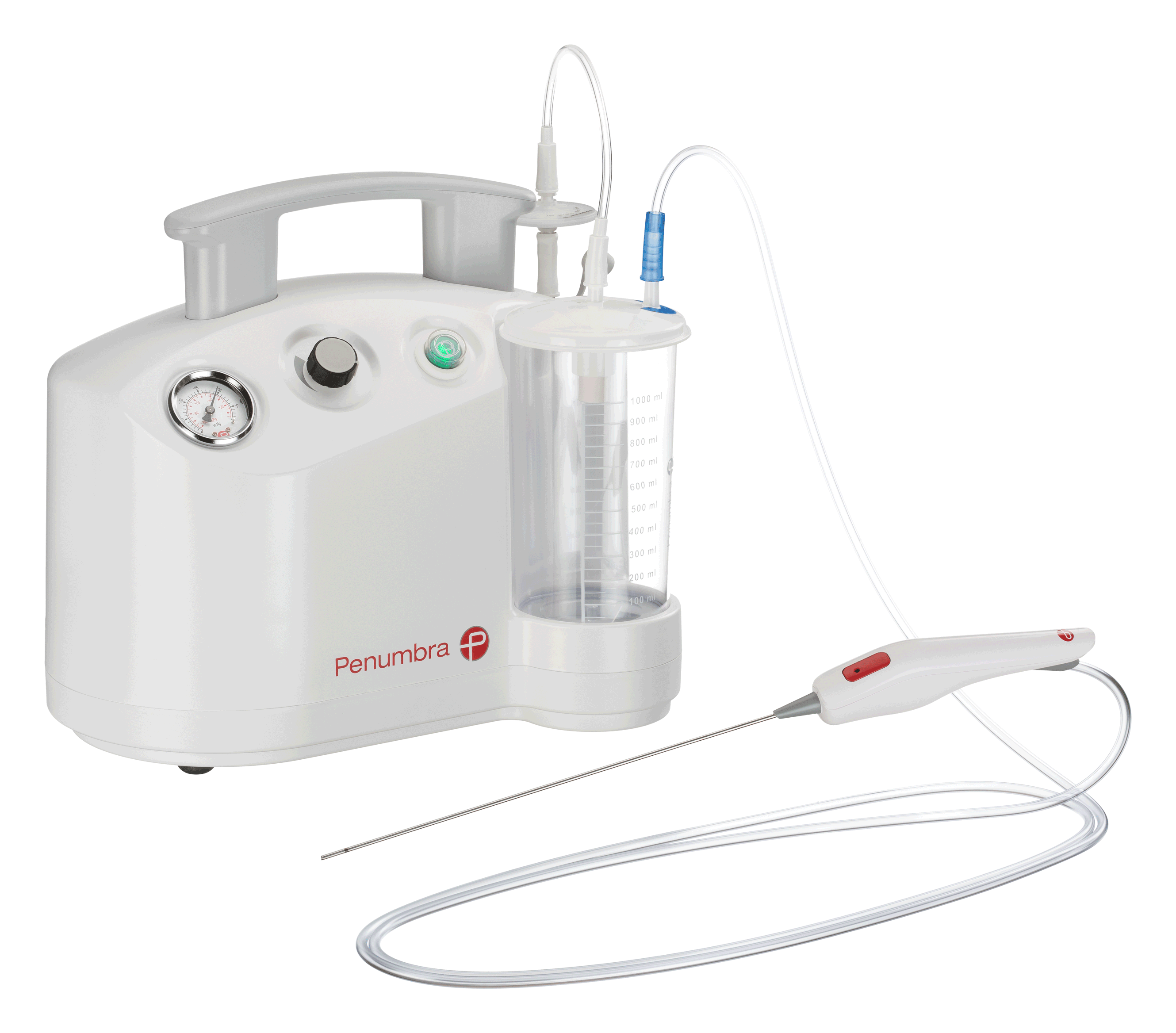
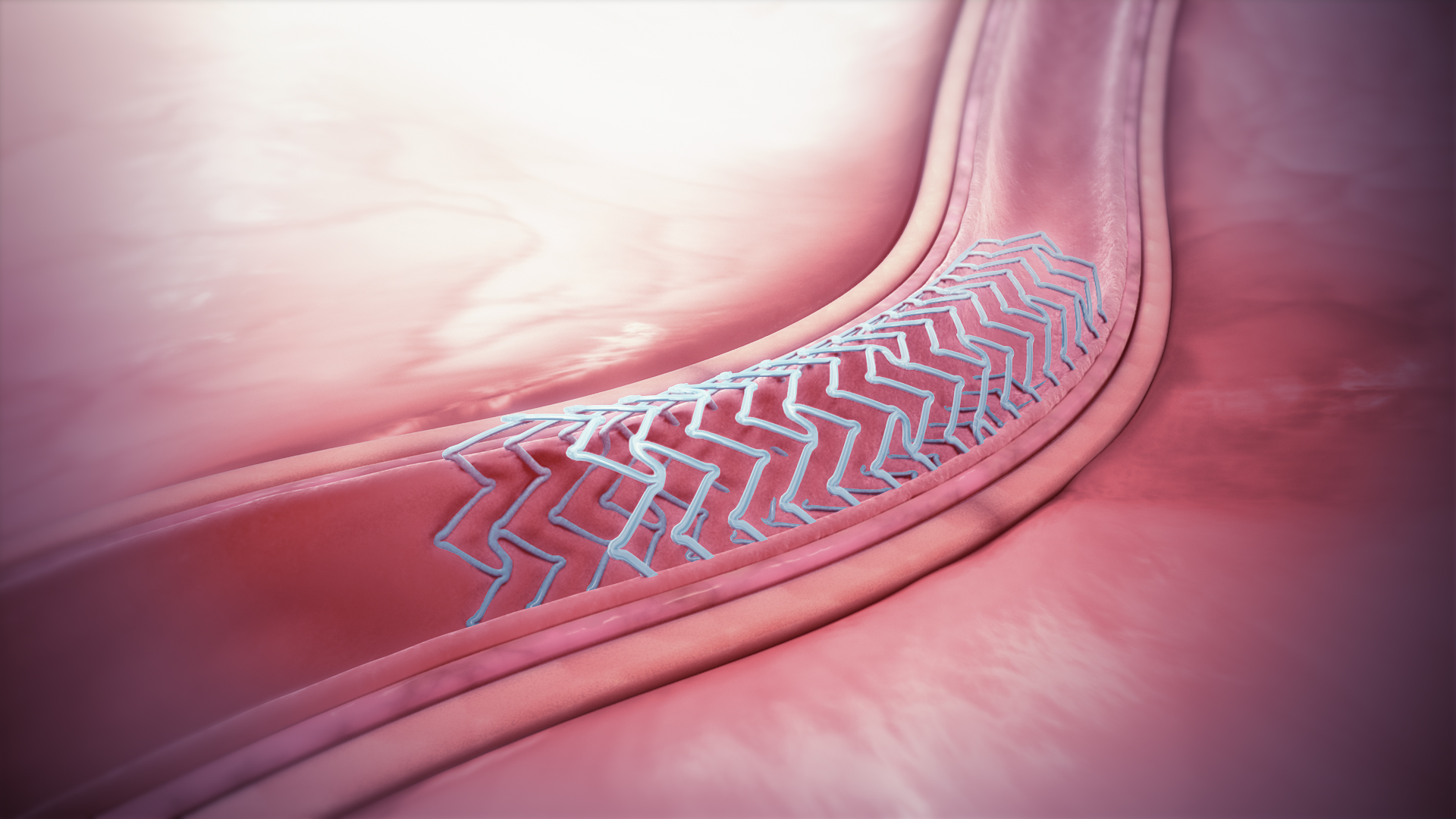
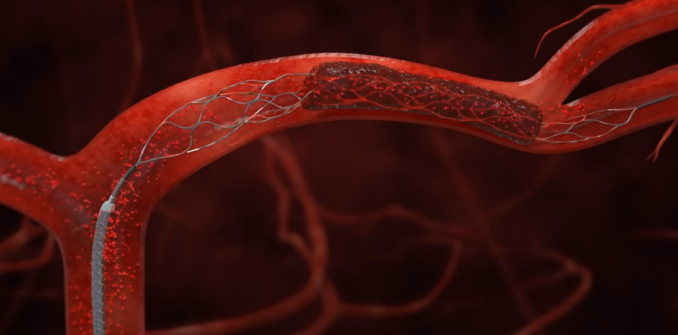
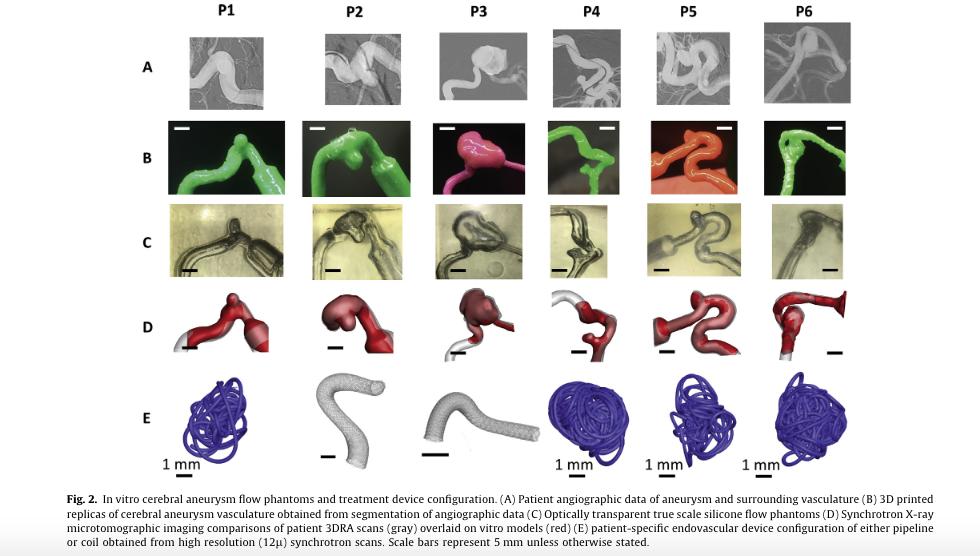
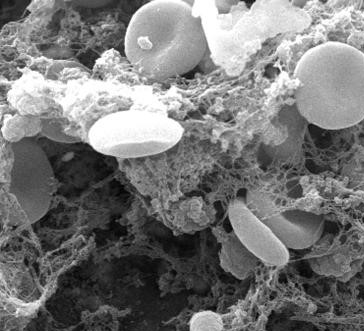
DURING:
Advance the treatment of stroke and neurological conditions through computational surgical simulations and medical device development.
AFTER:
Improve quality-of-life for our patients after they leave the hospital through addressing the medical and mental health burden following stroke and other neurological conditions.